Relevance:
Sociology: Women Issues: Emerging issues: ageing, sex ratios, child and infant mortality, reproductive health.
Context:
What happens when an expectant mother’s in-person social network shrinks or disappears overnight?
For the millions of women who celebrated their first Mother’s Day in May 2021, their transition into motherhood occurred in the shadow of the novel coronavirus disease.
Preparing for childbirth can be joyful and exciting, but COVID-19 restrictions disrupted many women’s prenatal care and forced some mothers to deliver their infants, without partner or family support. Others faced separation from their newborns immediately after birth.
Expectant parents also missed out on many celebrations and rituals that commemorate the transition into parenthood: baby showers, bris and christening ceremonies, neighbors dropping by with a meal, or grandparents traveling to meet the newest family member.
Over the past seven years, studies found that new parents, following couples from pregnancy across the first year postpartum. COVID-19 lockdowns last spring stopped our in-person data collection when our campus closed. But even as it stopped our usual research in its tracks, the pandemic created an opportunity to investigate a unique form of prenatal stress in real time.
Effects of prenatal stress can last throughout life
A tragic natural experiment helped spark study in the field researchers call “fetal origins of adult disease,” which explores links between pregnancy stress and later health.
At the tail end of World War II, the Nazi army cut off food supplies to the Netherlands, plunging the country into famine during the winter of 1944-1945. Babies in utero during what became known as the “Dutch Hunger Winter” showed lifelong differences in cardiometabolic health.
Because this was a clearly demarcated period of starvation, it even allowed researchers to investigate trimester-specific effects, finding that babies exposed to famine early in pregnancy showed outcomes different from those exposed late in pregnancy.
The COVID-19 pandemic shares many similarities with these events, including widespread loss of life. But it’s also unique. Communities often unite to grieve and rebuild after natural disasters.
The need to maintain social distance during the pandemic kept many people isolated from one another — especially many pregnant women, a high-risk population that may have elected to stick with stricter social distancing measures.
What happens when an expectant mother’s in-person social network shrinks or disappears overnight?
Social connection, mental health and COVID-19
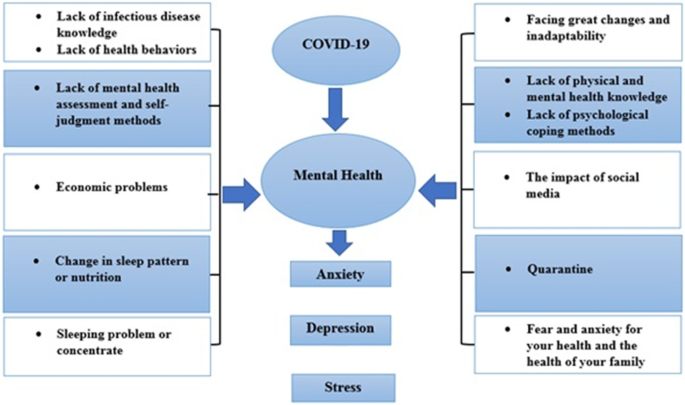
Scientists know social support buffers the risk for mental health problems in mothers. So our lab wondered how the sudden isolation of lockdowns — coupled with the economic and health worries of the pandemic — might affect pregnant women.
Only about five per cent of the pregnant women who responded to our survey had a suspected or confirmed case of COVID-19 as of spring 2020, and a similar number — 4.7 per cent — had experienced the death of someone close to them due to the pandemic.
However, 97 per cent reported that their community had issued a stay-at-home or shelter-in-place order. Moreover, 61 per cent of women reported that the pandemic had had “very” or “somewhat” negative impacts on their social relationships.
A majority of women estimated that at the time of the survey they had much less contact than before the start of the pandemic with neighbors and community members, co-workers, close friends and family members.
On the other hand, 42 per cent reported much more time spent with their partner than before the pandemic.
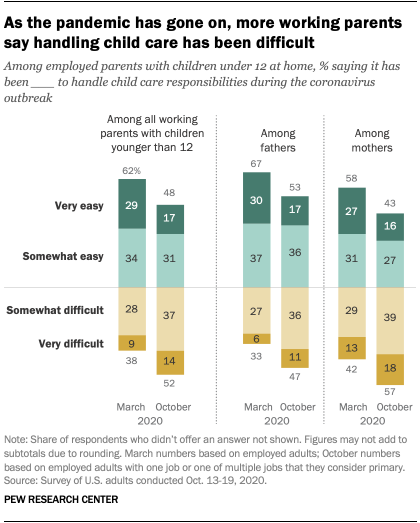
These changes in social contact appeared to take a mental health toll: almost two-thirds of respondents said they had experienced at least some loneliness over the previous week.
A similar number felt more lonely than usual because of the pandemic. Moreover, about three-fourths of our sample reported that the COVID-19 pandemic had an overall negative effect on their mental health.
To investigate further, we asked our respondents the questions on the Beck Depression Inventory, a tool that mental health care providers use to assess symptoms of depression.
The average score for pregnant women in our sample was higher than the threshold that clinicians typically use as an indicator for depression.
Half of the women in the sample reported clinically significant symptoms of depression. Similarly, more than half — 62 per cent — said they were experiencing clinically significant anxiety symptoms. These proportions are more than twice as high as what we’ve seen in our pre-pandemic sample.

COVID-19 stress could have long-term effects
It remains to be seen whether the stress of the pandemic’s first wave will have enduring mental health effects.
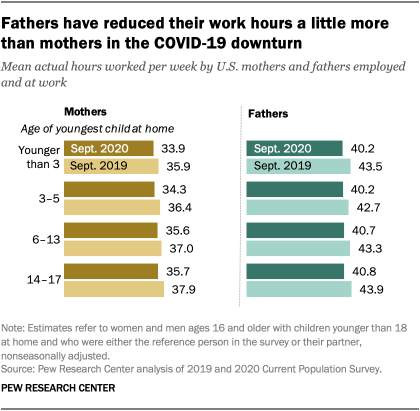
Some new mothers experienced silver linings of the pandemic, like greater ability to work from home after birth and sustain a breastfeeding relationship. At the same time, the pandemic took a greater toll on communities already affected by structural racism and poverty.
Research might find different trajectories of mental health, with pandemic lockdowns exacerbating some risk factors while perhaps exerting protective effects on other families.
In the meantime, our first batch of results suggests that these pandemic infants and their parents are a special population to follow into the future.
Currently pregnant women may face an easier transition into parenthood now that delivery-room restrictions have eased and social routines are returning to normal. But uncertainty, fear and grief from the many losses of the pandemic may linger even as the world reopens.
Compelling evidence suggests that counseling interventions such as talk therapy can not only relieve but also prevent mood disorders in the period immediately before and after birth.
Situations in which primary care and mental health care are integrated and expectant mothers can access psychotherapy through their OB-GYN practices can help treatments reach mothers most in need.
The pandemic eased many barriers to telehealth, as health care providers shifted to online visits; this format may also show promise reaching families who are still reluctant to make in-person visits.
We are continuing to follow our participants at three, six and 12 months after their baby’s birth to see how their mental health changes over time, with plans to extend the follow-up past the first year.
Although infants born in 2020 may not remember the pandemic firsthand, its effects may shape their early lives in ways that we are just beginning to measure.