COVID-19 & Changing Class Character Creating New Borders and Inequalities
Relevance: Sociology: Stratification and Mobility: (a) Concepts- equality, inequality, hierarchy, exclusion, poverty and deprivation. Paper II: Social Structure: (i) Rural and Agrarian Social Structure: (iv) Social Classes in India: (a) Agrarian class structure. (b) Industrial class structure. (c) Middle classes in India. & G.S paper I: Society and social issues
CONTEXT
With the extension of the lockdown in India came the news of a spike in the rate of COVID-19 infections. Just as the country is getting ready for life beyond lockdowns, the news of rising infections brings a fresh wave of fear and uncertainty..
The infection was now no longer restricted to the richer or creamier layers of society who travel or study abroad. The fear of infection was now from the poor and the marginalised.
Shifting class character of the infection
The shift in the class character of infection has happened repeatedly in the past. Tuberculosis was controlled much before the advent of any treatment though differences in the living conditions of those affected. The image of TB as a fashionable disease of the upper class soon changed to that of those living in squalid conditions in the mid and late 19th century in England.
The poor continued to be at risk while the more affluent who had the disease could go for long recovery retreats to sanatoria. Much later in India, polio continued to cling on to areas where the poor lived with little access to potable water and sanitation. Years of implementing a high-intensity vaccine programme have led to the elimination of polio, but drinking water and sanitation continue to be inaccessible to millions in the country even now.
What is clear is that the nature of the “vulnerable population”, or those at risk of the infection, has changed since the first cases were identified in February 2020. Initially, one heard incidents of how people returning to India from abroad were facing long queues before immigration as they were screened for possible infections.
By mid-March, the fear of infection had percolated into many upper-middle-class neighbourhoods and in many cities, the police came enquiring about visitors from abroad. Many Resident Welfare Associations were asked by the government to monitor the quarantine of other residents. In the six or more weeks since the first lockdown was announced the situation has changed.
A new category of ‘containment’ zone has now been created to identify a higher-level threat. The maps of containment zones, as evident from maps of Delhi and Kolkata, show how such neighbourhoods are distributed in these two cities. Kolkata has an even distribution of poor neighbourhoods while such neighbourhoods are towards the periphery in Delhi.
Changing patterns of spread of the infection
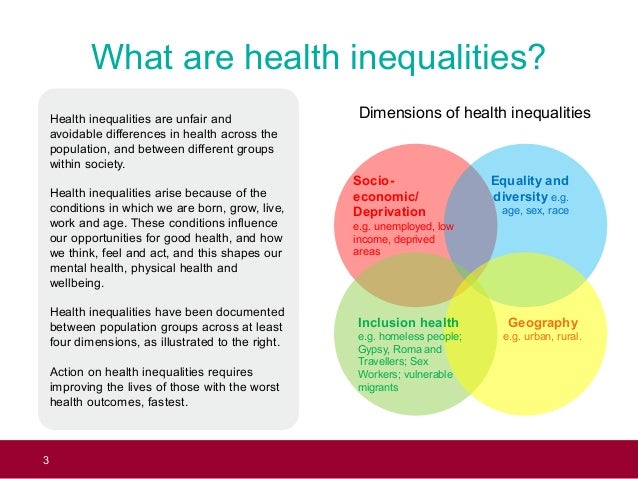
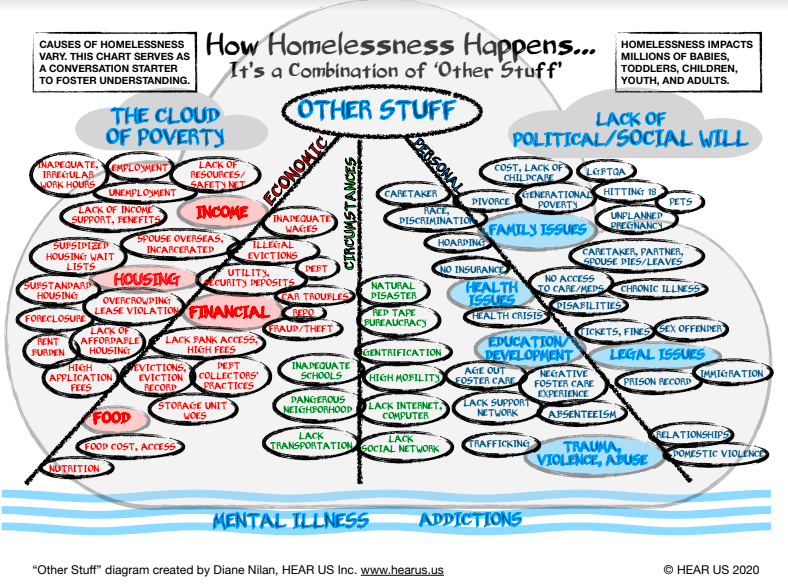
The further spread of COVID-19 in India must be considered in the context of the changing socio-economic pattern of infection and the larger socio-economic reality of India. The containment zone maps are likely to show increasing clusters of infections that overlaps with slums and other neighbourhoods that are inhabited by the poor and minority communities. These communities will be marked as ‘carriers’ and threats and therapeutic social distancing will lead to a much harder form of exclusion. A new form of differentiated spread will take place outside and within these increasingly hardening borders.
India is a deeply divided society. Economic inequality has increased in the last couple of decades. Despite having the fifth largest economy of the world, India’s rank on the Human Development Index (HDI) is a low 129 ( out of 189 countries). On the Global Hunger Index India ranks 102 (out of 117 countries) and is below all its neighbours (Afghanistan is not ranked). Gender inequality is high and India is ranked 122 (out of 162 countries) in the Gender Inequality Index.
Data from the National Crime Records Bureau and a report on social hostilities by the Pew Research Centre show that crimes of intolerance based on caste and religion are also very high. Within this already complex social reality, we now have an increasing perception that certain communities are vulnerable to the infection and can spread it more.
Since keeping a safe distance is the only general means of protection, the creation of hard borders will lead to new ways of policing or guarding these borders, allowing regulated entry and exit. The more affluent will maintain their safety by regulating their contact with the multiple service providers who meet their needs and keep the wheels of the economy running.

Sociologists have been using the term ‘bordering’ as a verb, indicating various measures which regulate the creation and passage between social and political barriers. The process was begun by setting up barriers around the Containment Zones.
The Aarogya Setu app that has been developed for contact tracing is being pushed for maximum coverage, and there is discussion on a ‘COVID passport’. Such instruments or permits and licenses may become essential for ensuring passage across these new ‘borders’, and while the affluent will keep themselves safe and the virus will be left to circulate within closed and densely populated spaces.
Need for a differentiated response
While the entire country has suffered considerably because of the virus, the recovery and reorganisation processes may be different for different population groups.
The urban middle class and those above faced the brunt of the first wave of infections and have probably benefited the most from the lockdown, containment and social distancing strategies that were the first line of defence. As the infection moves into different spaces, the ability of the communities living in those spaces to access appropriate preventive and curative health services becomes different.
The urban poor probably have the most fragmented and poorly regulated healthcare system. Urban India has a high concentration of the doctors and hospitals in the country with nearly 60% of all health workers working where only 30% of the population resides.
However, the urban poor are mostly served by less competent and less trained doctors. The poor face many social and economic barriers. A high density of population, lack of public health-related infrastructures like sewerage systems or piped water adds additional layers of risk to infection. The impact can be particularly severe where prevention requires physical distancing and frequent washing of hands with soap and water.

What happens in rural India now that the migrants are all returning home needs to be observed carefully. A preliminary study in Dungarpur, Rajasthan shows that returning migrants did not bring home the infection. The study highlights the different worlds that are inhabited by poor migrant labourers and the richer communities who travel abroad, calling it ‘enforced social distancing’.
The rural health system with few doctors and even fewer specialists has also been disrupted. In many districts, the larger hospitals have been kept ready for managing COVID-19 infections by sequestering beds. This also means that routine cases have had to suffer.
Rural India also has a growing number of private hospitals, but overall, the role and response of the private sector to COVID-19 has been extremely limited. Now that the probability of infections travelling to the rural areas is high it is important to plan appropriate health care responses which are not just based on fear, suspicion, and isolation.
Moving forward
Pandemics are known to facilitate large-scale social change processes. The feudal order in Europe had suffered a severe setback due to the Black Death in the fourteenth century because of the acute shortage of labour. Overall living conditions improved as wages increased and rents were driven down.
In India, opposition by local leaders to the strict measures of containment enforced by colonial rulers during the Plague through the same Epidemic Diseases Act 1897 – which is also being enforced today – gave a fillip to the nationalist movement.
Bal Gangadhar Tilak wrote against it in the newspaper Kesari and was sentenced to prison for 18 months. Inspired by Tilak the Chapekar brothers assassinated the ICS officer and Plague Commissioner of Pune, W.C. Rand and were subsequently hanged.
During the flu epidemic of 1918, the difference in mortality among the ruling British and the natives was vast, a pattern that could be replicated with COVID-19 if class differences are considered. The government response was found wanting and may have contributed to energising the nationalist movements and civil society responses.
How we live with COVID-19 in India will not only depend upon how the economy is re-energised or the health care system is organised. It will also depend upon how social relations are restructured.
In Germany, where there is strong social security, the government has announced that if companies reduce their workforce, the employees thus affected will continue to receive 60 – 67% of their earlier income as ‘short-time work allowance’ and in addition they would continue to receive their Social Security support.
In India, on the other hand, states have already started announcing the suspension of labour laws for stimulating the economy, which will add to the vulnerability that the poor already face.
The current approach to managing the pandemic, both by the government and the media has caused widespread fear and panic and new ways of stigmatisation and discrimination. While the need to keep a distance, wear masks, wash one’s hands regularly and not touch the mouth, nose or eyes is important, there has been little in the way of reassurance and better ways of coping and survival have not been provided. COVID-19, while being very contagious is not very deadly or lethal.
Research shows that not all coronavirus infections turn severe. Similarly, many who do show symptoms do not need hospitalisation. And a large proportion of those who do require hospitalisation recover and return home. The chances of survival even with infection, far outweigh, that of death. With protection and caution, the chances for infection too can be reduced.
The continuous message of fear from infection, disease and death that is emanating from the authorities and the media must change immediately as we develop mechanisms for coping and revitalising our lives. It is true that this road to recovery is going to be a long one, but we need to be prepared with our maps and compass.
The least we can do is take responsibility not only for our own safety and that of others but also ensure that all those around us whose lives are intrinsically linked to our own are treated with respect. Safety, dignity, and solidarity need to underpin all efforts aimed at rebuilding our future, either through government action or by us individuals and fellow citizens.

For more such notes, Articles, News & Views Join our Telegram Channel.
Click the link below to see the details about the UPSC –Civils courses offered by Triumph IAS. https://triumphias.com/pages-all-courses.php