Relevance: Mains: G.S paper II: Polity: Governance: Health
Context:
- The Centre brings virtually “all” medical devices under regulation for quality and safety.
• A gazette notification was issued to this effect on February 11, bringing all devices under the scope of Section 3 (b) of the Drugs and Cosmetics Act, 1940, which pertains to medical devices.
Present scenario:
- At present, over 35 devices are regulated or notified under the Medical Devices Rules, which came into force two years ago.
• The new categories of devices are likely to be notified from April this year. They will come under regulation after a period of 30-42 months.
• The domestic industry in particular has been given this window of adjustment to meet the required standards, the grace period rising with the levels of risk of the device.
• The nebulisers, blood-pressure monitoring devices, glucometers, disinfectants and insecticides, and digital thermometers, notified earlier as low risk devices, are likely to come under regulation from January 1, 2021.
• The high risk devices such as implants, CT scan equipment, MRI equipment, X-Ray machines, dialysis machines, also notified earlier, may come under the new regime from April 2021.
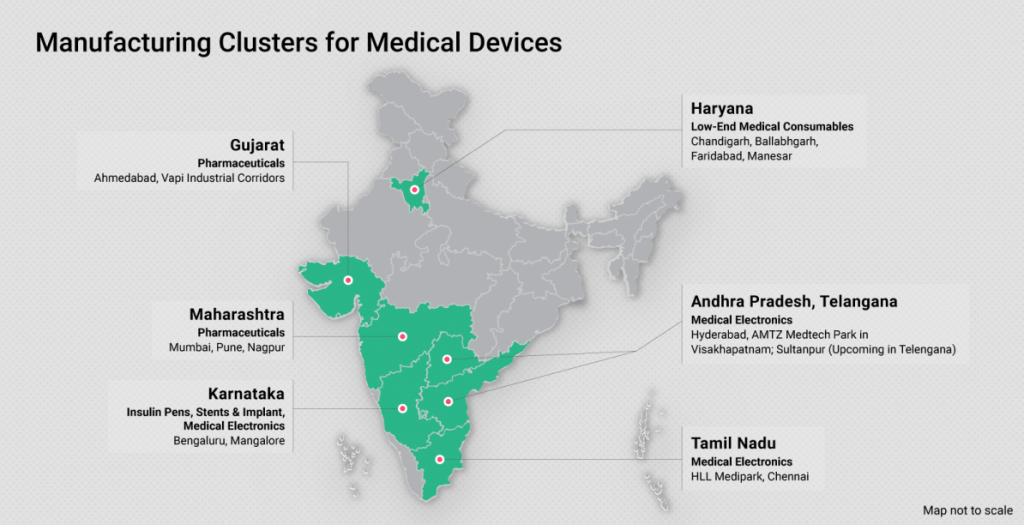
Boosting domestic medical equipment sector:
- In another boost to the domestic medical equipment sector, many of whom are MSMEs, the Centre has imposed a health cess on imported medical devices, with exceptions in the case of life-saving equipment.
• Any cess is, in principle, to be opposed, a levy in this case, coupled with the application of the Medical Devices Rules across the board, is expected to improve the competitiveness of the domestic industry.
• About 70 per cent of India’s ₹70,000-crore medical devices market is dominated by imports, with US and EU being key suppliers.
Enhance capabilities in regulation:
- A NITI Aayog Bill is in the works for effective regulation of medical devices, in the process removing them from the Drugs and Cosmetics Act.
• This might be necessary in view of the fact that drugs and devices are quite dissimilar in nature. It is also worth looking at whether quality certification of imported devices is to be accepted under all circumstances, without subjecting them to trials in the Indian context.
• The Johnson and Johnson hip transplant episode is instructive here. Norms for operational trials should be defined, and a sample size that is too small may not be reliable.
• The penal provisions should be applied with respect to the risk of a product, and not across the board. The most serious issue with regulating medical devices pertains to the lack of data.
• This is despite a ‘materio-vigilance programme’ having been in force since July 2015 to collect data through ‘material device adverse event monitoring centres’.
Conclusion:
- A move to create a ‘national registry’ of surgeons, as in the UK, should be expedited, with the Centre taking the lead.