Relevance: Sociology: Poverty, deprivation and inequalities. & G.S paper I: Society and Social Issues & G.S paper II: Governance: Health

Introduction
Five years into the 2030 Agenda, it is time to assess progress and to question whether continuing efforts implemented thus far will allow countries to reach SDG 2 targets.
For this reason, this year’s report complements the usual assessment of the state of food security and nutrition in the world with projections of what the world may look like in 2030 if trends of the last decade continue.
Importantly, as the COVID-19 pandemic continues to evolve, this report attempts to foresee some of the impacts of this global pandemic on food security and nutrition.
However, given that the full extent of the devastation that COVID-19 will cause is still largely unknown, it is important to recognize that any assessment at this stage is subject to a high degree of uncertainty and should be interpreted with caution.
Progress towards hunger and food insecurity targets The three most recent editions of this report already presented evidence that the decades-long decline in hunger in the world, as measured using the prevalence of undernourishment (PoU), had unfortunately ended.
Additional evidence and several important data updates, including a revision of the entire PoU series for China back to 2000, show that almost 690 million people in the world (8.9 percent of the world population) are estimated to have been undernourished in 2019.
Revision in light of the new data, which results in a parallel downward shift of the entire global PoU series, confirms the conclusion of past editions of this report: the number of people affected by hunger in the world continues to increase slowly.
This trend started in 2014 and extends to 2019. There are nearly 60 million more undernourished people now than in 2014, when the prevalence was 8.6 percent – up by 10 million people between 2018 and 2019.
The reasons for the observed increase of the last few years are multiple. Much of the recent increase in food insecurity can be attributed to the greater number of conflicts, often exacerbated by climate-related shocks. Even in some peaceful settings, food security has deteriorated as a result of economic slowdowns threatening access to food for the poor. The evidence also reveals that the world is not on track to achieve the SDG 2.1 Zero Hunger target by 2030.
Combined projections of recent trends in the size and composition of the population, in the total food availability, and in the degree of inequality in food access point to an increase of the PoU by almost 1 percentage point. As a result, the global number of undernourished people in 2030 would exceed 840 million. The PoU in Africa was 19.1 percent of the population in 2019, or more than 250 million undernourished people, up from 17.6 percent in 2014.
This prevalence is more than twice the world average (8.9 percent) and is the highest among all regions. Asia is home to more than half of the total undernourished people in the world – an estimated 381 million people in 2019. Yet, the PoU in the population for the region is 8.3 percent, below the world average (8.9 percent), and less than half of that of Africa. Asia has shown progress in reducing the number of hungry people in recent years, down by 8 million since 2015. In Latin America and the Caribbean, the PoU was 7.4 percent in 2019, below the world prevalence of 8.9 percent, which still translates into almost 48 million undernourished people. The region has seen a rise in hunger in the past few years, with the number of undernourished people increasing by 9 million between 2015 and 2019.

Overall, and without considering the effects of COVID-19, projected trends in undernourishment would change the geographic distribution of world hunger dramatically. While Asia would still be home to almost 330 million hungry people in 2030, its share of the world’s hunger would shrink substantially.
Africa would overtake Asia to become the region with the highest number of undernourished people (433 million), accounting for 51.5 percent of the total. At the time of this writing, the COVID-19 pandemic was spreading across the globe, clearly posing a serious threat to food security. Preliminary assessments based on the latest available global economic outlooks suggest that the COVID-19 pandemic may add between 83 and 132 million people to the total number of undernourished in the world in 2020 depending on the economic growth scenario (losses ranging from 4.9 to 10 percentage points in global GDP growth).

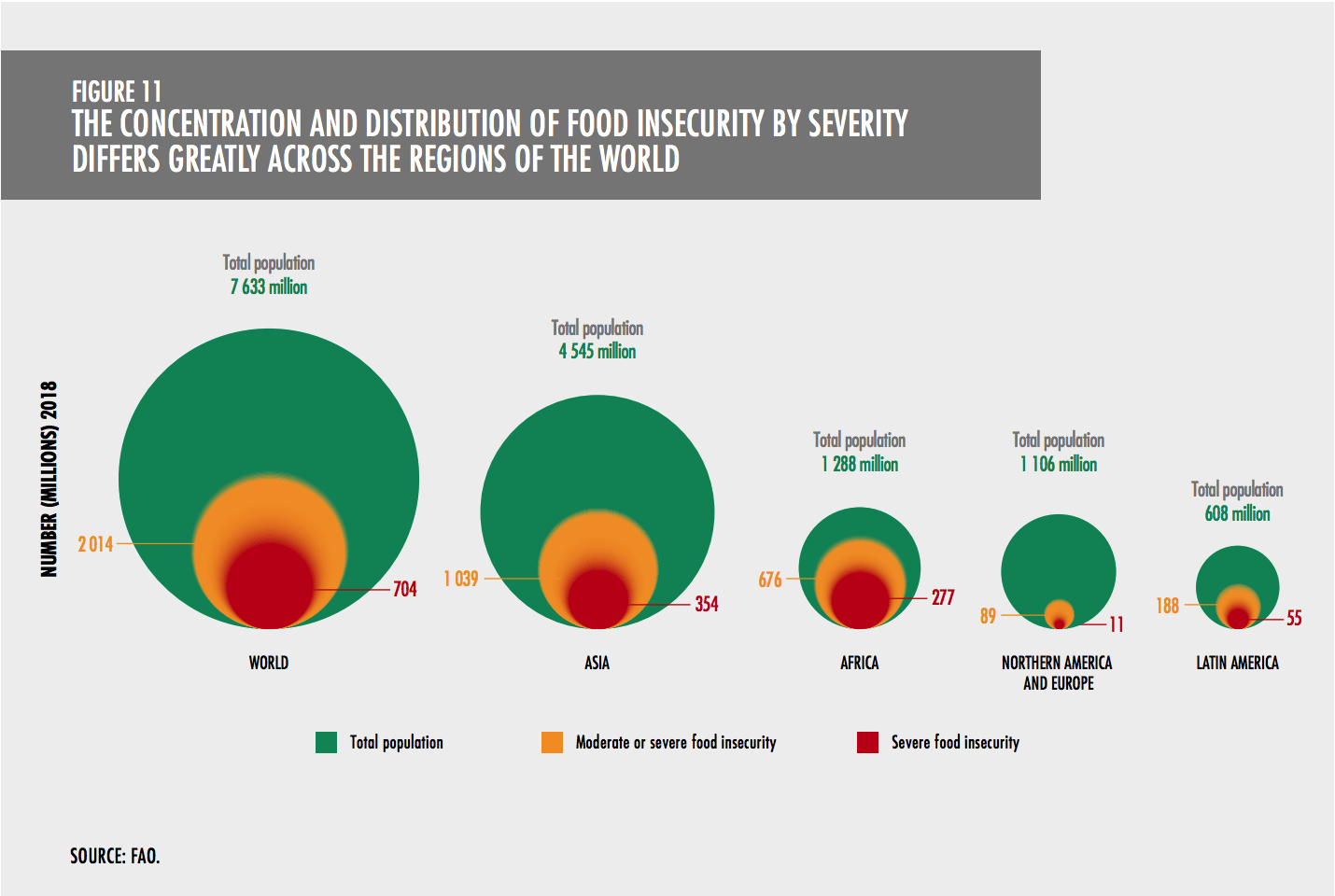
The expected recovery in 2021 would bring the number of undernourished down but still above what was projected in a scenario without the pandemic. Again, it is important to recognize that any assessment at this stage is subject to a high degree of uncertainty and should be interpreted with caution. Latest estimates suggest that 9.7 percent of the world population (slightly less than 750 million people) was exposed to severe levels of food insecurity in 2019. In all regions of the world except Northern America and Europe, the prevalence of severe food insecurity has increased from 2014 to 2019.
This is also broadly consistent with recent trends in the PoU in the world and across regions, with the partial exception of Asia. While the 746 million people facing severe food insecurity are of utmost concern, an additional 16 percent of the world population, or more than 1.25 billion people, have experienced food insecurity at moderate levels. People who are moderately food insecure do not have regular access to nutritious and sufficient food, even if not necessarily suffering from hunger.
The prevalence of both moderate and severe levels of food insecurity (SDG Indicator 2.1.2) is estimated to be 25.9 percent in 2019 for the world as a whole. This translates into a total of 2 billion people. Total food insecurity (moderate or severe) has consistently increased at the global level since 2014, mostly because of the increase in moderate food insecurity. Although Africa is where the highest levels of total food insecurity are observed, it is in Latin America and the Caribbean where food insecurity is rising the fastest: from 22.9 percent in 2014 to 31.7 percent in 2019, due to a sharp increase in South America.
In terms of the distribution of total food insecure (moderate or severe) people in the world, out of the 2 billion people suffering from food insecurity, 1.03 billion are in Asia, 675 million in Africa, 205 million in Latin America and the Caribbean, 88 million in Northern America and Europe, and 5.9 million in Oceania. At the global level, the prevalence of food insecurity at moderate or severe level, and severe level only, is higher among women than men.
The gender gap in accessing food increased from 2018 to 2019, particularly at the moderate or severe level. Progress towards global nutrition targets Worldwide, the prevalence of child stunting in 2019 was 21.3 percent, or 144 million children.
Although there has been some progress, rates of stunting reduction are far below what is needed to reach the World Health Assembly (WHA) target for 2025 and the SDG target for 2030. If recent trends continue, these targets will only be achieved in 2035 and 2043, respectively. In 2019, more than nine out of ten stunted children lived in Africa or Asia, representing 40 percent and 54 percent of all stunted children in the world, respectively.

Most regions have made some progress in reducing stunting between 2012 and 2019 but not at the rate needed to achieve the 2025 and 2030 targets. Globally, stunting estimates vary by wealth. Children from the poorest wealth quintile had a stunting prevalence that was more than double that of children from the richest quintile. The global prevalence of overweight among children under 5 years of age has not improved, going from 5.3 percent in 2012 to 5.6 percent, or 38.3 million children, in 2019. Of these, 24 percent lived in Africa and 45 percent in Asia. Australia and New Zealand is the only subregion with a very high prevalence (20.7 percent). Southern Africa (12.7 percent) and Northern Africa (11.3 percent) have prevalences considered high. Globally, 6.9 percent of children under 5 (47 million) were affected by wasting in 2019 – a figure significantly above the 2025 target (5 percent) and the 2030 target (3 percent) for this indicator.
Worldwide, 14.6 percent of infants were born with low birthweight (less than 2 500 g) in 2015. The trends for this indicator at global and regional level show that some progress has been made in recent years, but not enough to achieve the target of a 30 percent reduction in low birthweight by 2025 or even by 2030. Globally, as of 2019, it is estimated that 44 percent of infants aged less than six months were exclusively breastfed. Currently, the world is on track to achieve the 2025 target of at least 50 percent of babies younger than six months being exclusively breastfed. If additional efforts are not made, however, the global target for 2030 of at least 70 percent will not be achieved before 2038. Most subregions are making at least some progress, except Eastern Asia and the Caribbean.
If the Eastern Africa, Central Asia and Southern Asia subregions maintain their current rates of progress, they will reach the targets set for both 2025 and 2030. Adult obesity continues to rise, from 11.8 percent in 2012 to 13.1 percent in 2016 and is not on track to reach the global target to halt the rise in adult obesity by 2025. If the prevalence continues to increase by 2.6 percent per year, adult obesity will increase by 40 percent by 2025, compared to the 2012 level. All subregions show increasing trends in the prevalence of adult obesity between 2012 and 2016. The critical link between food security and nutrition outcomes: food consumption and diet quality Diet quality comprises four key aspects: variety/ diversity, adequacy, moderation and overall balance. According to WHO, a healthy diet protects against malnutrition in all its forms, as well as non-communicable diseases (NCDs) such as diabetes, heart disease, stroke and cancer. It contains a balanced, diverse and appropriate selection of foods eaten over a period of time.
In addition, a healthy diet ensures that a person’s needs for macronutrients (proteins, fats and carbohydrates including dietary fibres) and essential micronutrients (vitamins and minerals) are met, specific to their gender, age, physical activity level and physiological state. Healthy diets include less than 30 percent of total energy intake from fats, with a shift in fat consumption away from saturated fats to unsaturated fats and the elimination of industrial trans fats; less than 10 percent of total energy intake from free sugars (preferably less than 5 percent); consumption of at least 400 g of fruits and vegetables per day; and not more than 5 g per day of salt (to be iodized). While the exact make-up of a healthy diet varies depending on individual characteristics, as well as cultural context, locally available foods and dietary customs, the basic principles of what constitutes a healthy diet are the same. Global assessment of food consumption and diet quality poses many challenges. To date, there is no single, validated composite index to measure the multiple dimensions of diet quality across all countries. Data on food availability at the country level show large discrepancies in the per capita availability of foods from different food groups across different country income groups. Low-income- and lower-middle-income countries rely heavily on staple foods like cereals, roots, tubers and plantains. Overall, the availability of staple foods for the world has changed little between 2000 and 2017. Availability of roots, tubers and plantains increased in lower-middle-income countries, driven by a rise in Africa, whereas it decreased in high-income countries. In low-income countries, cereals, roots, tubers and plantains represent nearly 60 percent of all food available in 2017. This percentage decreases gradually with country income groups, down to 22 percent in high-income countries.
The world average availability of fruits and vegetables increased; however, only in Asia, and globally in upper-middle-income countries, are there enough fruits and vegetables available to meet the FAO/WHO recommendation of consuming a minimum of 400 g per day. Availability of animal source foods overall is highest in high-income countries, but it is growing rapidly in upper-middle-income countries. Most of the global increases in animal source foods were observed in lower- and upper-middle-income countries. Asia showed the largest increase in the total amount of animal source foods available. The contribution from animal source foods varies with the country income group. It is higher in high-income countries (29 percent) compared to upper-middle- and lower-middle-income countries (20 percent), and lowest in low-income countries (11 percent). According to UNICEF, dietary diversity in infants and young children was low in the majority of the regions, with less than 40 percent of children meeting minimum dietary diversity in seven out of the eleven subregions. In addition, there are stark disparities in the prevalence of minimum dietary diversity by the place of residence (urban/rural) and wealth status. The prevalence of children eating foods from at least five out of eight food groups is on average 1.7 times higher among children living in urban households than in rural, and among those living in the richest households compared to the poorest. How does food insecurity affect what people eat? An analysis of dietary patterns according to levels of food insecurity found that diet quality worsens with increasing severity of food insecurity.
The ways in which moderately food insecure people modify their diets vary according to the income level of the country. In two lower-middle-income countries studied (Kenya and Sudan), there is a marked decrease in consumption of most food groups, and an increase in the share of staples in the diet. In two upper-middle-income countries examined (Mexico and Samoa), people who are moderately food insecure consume more foods that are typically cheaper on a per-calorie basis (cereals, roots, tubers and plantains), and consume lesser amounts of expensive foods (meat and dairy), compared with those who are food secure. Mexico in particular shows a decrease in fruit and dairy consumption as the severity of food insecurity increases. In summary, with ten years to go until 2030, the world is off track to achieve the SDG targets for hunger and malnutrition. After decades of long decline, the number of people suffering from hunger has been slowly increasing since 2014. Beyond hunger, a growing number of people have been forced to compromise on the quality and/or quantity of the food they consume, as reflected in the increase in moderate or severe food insecurity since 2014. Projections for 2030, even without considering the potential impact of COVID-19, serve as a warning that the current level of effort is not enough to reach Zero Hunger ten years from now. As for nutrition, progress is being made on decreasing child stunting and low birthweight and on increasing exclusive breastfeeding for the first six months of life. However, the prevalence of wasting is notably above the targets and the prevalence of both child overweight and adult obesity is increasing in almost all regions. COVID-19 is expected to exacerbate these trends, rendering vulnerable people even more vulnerable.
Increasing availability of and access to nutritious foods that comprise healthy diets must be a key component of stronger efforts to achieve the 2030 targets. The remaining years of the UN Decade of Action on Nutrition 2016–2025 present an opportunity for policymakers, civil society and the private sector to work together and accelerate efforts.
TRANSFORMING FOOD SYSTEMS TO DELIVER AFFORDABLE HEALTHY DIETS FOR ALL
As already highlighted above, diet quality is a critical link between food security and nutrition outcomes that needs to be present as part of all efforts to achieve the hunger, food security and nutrition targets of SDG 2. Meeting these targets will only be possible if we ensure that people have enough food to eat, and that what they are eating is nutritious. However, one of the biggest challenges to achieving this is the current cost and affordability of healthy diets, which is the focus of Part 2 of this report this year. The cost and affordability of healthy diets around the world New analysis presented in this report aims to determine whether the food system brings three levels of diet quality within reach of the poorest. The three diets chosen denote increasing levels of diet quality, starting from a basic energy sufficient diet meeting calorie needs, to a nutrient adequate diet and then a healthy diet, the latter including an estimation of recommended intake of more diversified and desirable food groups. As expected, the cost of the diet increases incrementally as the diet quality increases and this is true across all regions and country income groups. The cost of a healthy diet is 60 percent higher than the cost of the nutrient adequate diet, and almost 5 times the cost of the energy sufficient diet.
While most of the poor around the world can afford an energy sufficient diet, as defined here, they cannot afford either a nutrient adequate or a healthy diet. A healthy diet is far more expensive than the full value of the international poverty line of USD 1.90 PPP per day, let alone the portion of the poverty line that can credibly be reserved for food (63 percent), to end up with a threshold of USD 1.20 PPP per day. When comparing its cost to household food expenditure, on average a healthy diet is affordable, with the cost representing 95 percent of average food expenditures per capita per day at the global level. Most striking is that the cost of a healthy diet exceeds national average food expenditures in most countries in the Global South. It is estimated that based on average estimated incomes more than 3 billion people in the world could not afford a healthy diet in 2017. Most of these people are found in Asia (1.9 billion) and Africa (965 million), although there are also millions that live in Latin America and the Caribbean (104.2 million), and in Northern America and Europe (18 million).
While the cost and affordability of diets varies around the world, across regions and in different development contexts, they may also vary within countries due to temporal and geographical factors, as well as variations in the nutritional needs of individuals across the life cycle. These within-country variations in cost are not captured in the above global and regional analysis – but evidence from case studies makes it clear such variations can be substantial.
The hidden health and environmental costs of what we eat Valuing the hidden costs (or negative externalities) associated with different diets could modify significantly our assessment of what is “affordable” from a broader societal perspective and reveal how dietary choices affect other SDGs. Two hidden costs that are most critical relate to the health (SDG 3) and climate-related (SDG 13) consequences of our dietary patterns and the food systems that support these. The health and environmental consequences of unbalanced and unhealthy diets translate into actual costs for individuals and society as a whole, such as increased medical costs and the costs of climate damage, among other environmental costs. New analysis for this report has estimated the health and climate-change costs of five different dietary patterns: one benchmark diet, representing current food consumption patterns, and four alternative healthy diet patterns that, although differing in the way they include foods from several groups and diversity within food groups, all include sustainability considerations.
The health impacts associated with poor diet quality are significant. Diets of poor quality are a principal contributor to the multiple burdens of malnutrition – stunting, wasting, micronutrient deficiencies, overweight and obesity and both undernutrition early in life and overweight and obesity are significant risk factors for NCDs. Unhealthy diets are also the leading risk factor for deaths from NCDs. In addition, increasing healthcare costs linked to increasing obesity rates are a trend across the world. Assuming that current food consumption patterns accommodate expected changes in income and population, as per in the benchmark scenario representing current food consumption patterns, health costs are projected to reach an average of USD 1.3 trillion in 2030. More than half (57 percent) of these are direct healthcare costs as they are associated with expenses related to treating the different diet-related diseases. The other part (43 percent) accounts for indirect costs, including losses in labour productivity (11 percent) and informal care (32 percent).
If, instead, any of the four alternative diet patterns used for the analyses are adopted (FLX, PSC, VEG, VGN), diet-related health costs dramatically decrease by USD 1.2–1.3 trillion, representing an average reduction of 95 percent of the diet-related health expenditures worldwide compared to the benchmark scenario in 2030. What people eat, and how that food is produced, not only affects their health, but also has major ramifications for the state of the environment and for climate change. The food system underpinning the world’s current dietary patterns is responsible for around 21–37 percent of total greenhouse gas (GHG) emissions, which reveals it to be a major driver of climate change, even without considering other environmental effects.
Most global and cross-country valuations of environmental impacts focus on GHG emissions, because data limitations hamper global cross-country comparisons of other important environmental impacts related to land use, energy and water use. This data limitation also affects this report’s own global analysis, which looks at the hidden climate-change costs by focusing exclusively on GHG emissions and their climate impacts. The diet-related social cost of GHG emissions related to current food consumption patterns are estimated to be around USD 1.7 trillion for 2030 for an emissions-stabilization scenario. Our analysis shows that adoption of any of the four alternative healthy diet patterns that include sustainability considerations could potentially contribute to significant reductions of the social costs of GHG emissions, ranging from USD 0.7 to USD 1.3 trillion across the four diets (41–74 percent) in 2030.
Managing trade-offs and exploiting synergies in the transition towards healthy diets that include sustainability considerations To achieve the dietary patterns for healthy diets that include sustainability considerations, large transformative changes in food systems will be needed at all levels. Given the large diversity of current food systems and wide discrepancies in food security and nutrition status across and within countries, there is no one-size-fits-all solution for countries to move from the status quo to achieving healthy diets and create synergies to reduce their environmental footprints.
Assessing the context-specific barriers, managing (and sometimes enduring) short-term and long-term trade-offs and exploiting synergies is critical. While the cost of the healthy diet is lower than current food consumption patterns when one considers health and climate-related externalities, in some contexts, there are other important indirect costs and trade-offs.
For countries where the food system not only provides food, but also drives the rural economy, it will be important to consider the impact of shifting to healthy diet patterns in terms of the livelihoods of smallholder farmers and the rural poor as well. In these cases, care must be taken to mitigate the negative impact on incomes and livelihoods as food systems transform to deliver affordable healthy diets. Many lower-income countries, where populations already suffer nutrient deficiencies, may need to increase their carbon footprint in order to first meet recommended dietary needs and nutrition targets, including those on undernutrition. On the other hand, other countries, especially upper-middle-income and high-income countries, where diet patterns exceed optimal energy requirements, and where people consume more animal source foods than required, will need to make major changes in their dietary practices and food environments as well as system-wide changes in food production and trade.
What is driving the cost of nutritious food?
To increase the affordability of healthy diets, the cost of nutritious foods must come down. Many factors determine the consumer price of nutritious food, from the point of production throughout the food supply chain, and also within the food environment when consumers engage with the food system to make decisions about acquiring, preparing and consuming foods.
Addressing low productivity in food production can be an effective way of raising the overall supply of food, including nutritious foods, by reducing food prices and rising incomes, especially for the poorer family farmers and smallholder producers in low-income and lower-middle-income countries, like farmers, pastoralists and fisherfolk. In addition to low productivity, insufficient diversification towards the production of horticultural products, legumes, small-scale fisheries, aquaculture, livestock and other nutritious food products also limits the supply of diverse and nutritious foods in markets, resulting in higher food prices.
Reducing pre-harvest and post-harvest losses in quantity and quality at the production level in the agriculture, fisheries and forestry sectors is an important starting point to reduce the cost of nutritious foods along the food supply chain, as this decreases the overall availability of these foods – while possibly contributing to environmental sustainability as well. Another important component of market infrastructure is the overall quality and efficiency of the national road and transportation network, which is critical in getting produce from the farm gate to markets at reasonable cost.
The distance to food marketplaces and the time required to prepare a healthy meal in times of rapid urbanization and increasing involvement of women in economic activities can also be seen as cost drivers because people who try to overcome them would have to accept an additional cost on top of the cost of food itself. Food and agricultural policies also have the power, either directly or indirectly, to affect the cost of food. In particular, the priorities of the food and agriculture policy framework illustrate the difficult balancing act required when choosing between actions in agriculture versus other sectors; among different government objectives (e.g. different fiscal policies); between benefits for producers, consumers and intermediaries; and even between different agricultural subsectors.
Trade policies affect the cost and affordability of healthy diets by altering the relative prices between imported and import-competing foods. Protectionary trade measures such as import tariffs, bans and quotas – together with input subsidy programmes – have often been embedded in self-sufficiency and import substitution strategies.
In low-income countries, this policy has protected and incentivized the domestic production of energy-dense foods such as rice and maize, but often at the detriment of vitamin- and micronutrient-rich products (i.e. fruits and vegetables). This can have an adverse effect on the affordability of more nutritious foods. Non-tariff measures, such as sanitary and phyto-sanitary measures (SPS) and technical barriers to trade (TBT) can also negatively affect the affordability of diets, as for example, exporters and importers may face additional costs to comply with regulatory requirements, driving up the cost of trade.
Last but not least, globalization has been accompanied by a massive growth of investments by transnational food corporations and rapidly increasing levels of food sold through supermarkets, referred to as the “supermarket revolution”. These developments represent a key aspect of the political economy that drive food systems transformation and influence the cost and affordability of food. Policies to reduce the cost of nutritious foods and ensure affordability of healthy diets Ten years remain to achieve the ambitious SDG targets within the current economic, social and political environment – an environment increasingly vulnerable to climate and other shocks, not to mention the unprecedented health, social and economic impacts of the COVID-19 pandemic.
With this short timeline, countries must identify and implement critical policy and investment changes that will transform their current food systems to ensure everybody can afford healthy diets that include sustainability considerations. Urgent action is needed, especially for the poorest in society, who face the greatest challenges. Reducing the cost of nutritious foods and increasing the affordability of healthy diets must start with a reorientation of agricultural priorities towards more nutrition-sensitive food and agricultural production.
Public expenditures will need to be stepped up to enable many of the policy decisions and investments needed to raise productivity, encourage diversification in food production and ensure that nutritious foods are made abundantly available. Policies that penalize food and agricultural production (through direct or indirect taxation) should be avoided, as they tend to have adverse effects on the production of nutritious foods.
Subsidy levels in the food and agriculture sectors should also be revisited, especially in low-income countries, to avoid taxation of nutritious foods. Policies should promote investment in irrigation infrastructure specifically targeting strengthened capacity for all-season vegetable production and other high-value commodities to increase availability of nutritious foods.
Likewise, national food and agricultural strategies and programmes should step up investment in research and development (R&D) to raise productivity of nutritious foods and help reduce their cost, while enhancing access to improved technologies, especially for family farmers and smallholder producers, to maintain adequate levels of profitability.
There is a need for stronger policies towards more nutrition-sensitive value chains. Key policy actions include investments in improved storage, processing and preservation to retain the nutritional value of food products, rather than investing in highly processed foods. Improving the national road network, as well as transport and market infrastructure, can go a long way to ensuring greater affordability of healthy diets. In addition to food storage, appropriate food handling and processing facilities are central to increasing efficiencies along the value chain for nutritious foods.
Policies and investments should also focus on reducing food losses, as this can increase affordability of nutritious foods in two ways. First, by focusing on the earlier (production) stages of the food supply chain, as this tends to boost supplies and hence reduce food prices at the farm gate. This is particularly important for the reduction of losses in perishable commodities, such as fruits and vegetables, dairy, fish and meat.
Second, by targeting the parts of the food supply chain where food losses are greatest, as this will more likely have a greater impact on reducing the cost of the targeted food item. The overall price effect will differ from one commodity to the next and also across countries. Trade and marketing policies aimed at decreasing the cost of food to consumers, while avoiding disincentives to the local production of nutritious foods, are often difficult to balance.
Nevertheless, the efficiency of internal trade and marketing mechanisms are possibly just as important as measures to support international trade – if not more – in determining the cost of healthy diets for both urban and rural consumers, while also ensuring that food safety standards are met. Policies aimed at reducing poverty and income inequality, while enhancing employment and income-generating activities, are key to raising people’s incomes and hence the affordability of healthy diets.
While there are important synergies between policies enhancing employment and reducing income inequality for increased food security and better nutrition, including social protection, these have been addressed in depth in the 2019 edition of this report.
In this edition of the report, the importance of nutrition-sensitive social protection policies is particularly highlighted. These types of policies are most appropriate to provide better access to nutritious foods to lower-income consumers and thus increase their affordability of healthy diets. It is important to strengthen nutrition-sensitive social protection mechanisms, ensuring they can support micronutrient supplementation where needed, as well as create healthy food environments by encouraging consumers to diversify their diets to reduce dependence on starchy staples, reduce consumption of foods high in fats, sugars and/or salt, and include more diverse, nutritious foods.
These mechanisms may include a number of policy tools, typically cash transfer programmes, but also in-kind transfers, school feeding programmes and subsidization of nutritious foods. These policies can be particularly important in the face of adversity, as we are seeing today during the COVID-19 pandemic.
Given different starting points and challenges in each country, as well as the potential trade-offs, a combination of complementary policy interventions towards reducing the cost of nutritious foods, while enhancing the affordability of healthy diets is likely to be more effective than any single policy measure. To achieve the healthy dietary patterns, large transformative changes in food systems will be needed at all levels and it is important to underscore that, although there are some overlaps, these changes go beyond the policy options and investments that are explicitly designed and implemented to reduce the cost of and increase the affordability of healthy diets. That is to say, other conditions must also be met, requiring a whole range of other policies that are more explicitly tailored to raise awareness and influence consumer behaviour in favour of healthy diets, possibly with important synergies for environmental sustainability.
For more such notes, Articles, News & Views Join our Telegram Channel.
Click the link below to see the details about the UPSC –Civils courses offered by Triumph IAS. https://triumphias.com/pages-all-courses.php