Relevance: Sociology: Women Empowerment: Women rights: Family planning & Population control: Patriarchy
Why in news?
- The Minister of State (Health and Family Welfare) has informed India’s modern contraceptive usage is 47.8% as per NFHS IV (2015-16).
Key highlights:
- Mission ParivarVikas- The Government has launched Mission Parivar Vikas on 10th November 2016 for substantially increasing access to contraceptives and family planning services in146 high fertility districts with Total Fertility Rate (TFR) of 3 and above in seven high focus states. These districts are from the states of Uttar Pradesh (57), Bihar (37), Rajasthan (14), Madhya Pradesh (25), Chhattisgarh (2), Jharkhand (9) and Assam (2) that itself constitutes 44% of the country’s population.
- New Contraceptive Choices- New contraceptives viz. Injectable contraceptive (Antara program) and Centchroman (Chhaya) have been added to the existing basket of choices in 2015-16.
- A new method of IUCD insertion immediately after delivery i.e. post-partum IUCD (PPIUCD) has been introduced in 2010. PPIUCD incentive scheme has been operational wef 01.01.2014.
- Emphasis on Post pregnancy Family Planning services which includes promotion of Post-Partum and Post-Abortion contraception.
- Redesigned Contraceptive Packaging – The packaging for Condoms, OCPs and ECPs has been improved and redesigned since 2015 in order to increase the demand for these commodities.
- Family Planning Logistic Management and Information System (FP-LMIS): A dedicated software launched in 2017, to ensure smooth forecasting, procurement and distribution of family planning commodities across all the levels of health facilities.
- Appointment of dedicated RMNCH+A counselors at high case load facilities since 2013.
- Improved Demand generation activities through a holistic media campaign- 1st phase launched in 2015, and the present 2nd phase in 2016.
- Observation of World Population Day and fortnight from July 11 – July 24 to boost Family Planning efforts all over the country.
- Observation of Vasectomy Fortnight from November 21 – December 4 in an effort to enhance male participation and revitalize the NSV programme.
- Scheme for Home delivery of contraceptives by ASHAs at doorstep of beneficiaries launched in August 2011.
- Scheme for ASHAs to Ensure spacing in births launched on 16th May 2012-The scheme is being implemented in 18 states of the country (8 EAG, 8 North East, Gujarat and Haryana). Additionally the spacing component has been approved in West Bengal, Karnataka, AndhraPradesh, Telangana, Punjab, Maharashtra, Daman Diu and Dadra and Nagar Haveli.
- Scheme for provision of Pregnancy Testing Kits in the drug kits of ASHAs for use in communities. The Scheme was introduced in 2013.
- National Family Planning Indemnity Scheme (NFPIS) under which clients are insured in the eventualities of death, complication and failure following sterilization.The scheme was introduced in 2005 and implemented through an insurance company. It was revised in 2013 and is now being operated by the state governments directly with NHM funding.
- Compensation scheme for sterilization acceptors – Under the scheme MoHFW provides compensation for loss of wages to the beneficiary and also to the service provider (and team) for conducting sterilizations. The package was enhanced in November 2014 for 11 high focus high TFR states (8 EAG, Assam, Gujarat, Haryana), and further increased in November 2016 under Mission ParivarVikas.
- Clinical Outreach Teams (COT) Scheme – The scheme has been launched in 146 Mission ParivarVikas districts wef December 2017 for providing family planning services through mobile teams from accredited organizations in far-flung, underserved and geographically difficult areas.
- Ensuring quality of care in Family Planning services by establishing Quality Assurance Committees in all states and districts.
SOCIOLOGICAL PERSPECTIVE
FEMINIST PERSPECTIVE

Many societies have made the transition from high mortality and large family sizes to settings where most children survive, small families are desired, and most people control their fertility. In the early 1960s, the average woman could expect to have almost five children over her life, but now she can expect to have fewer than three children.
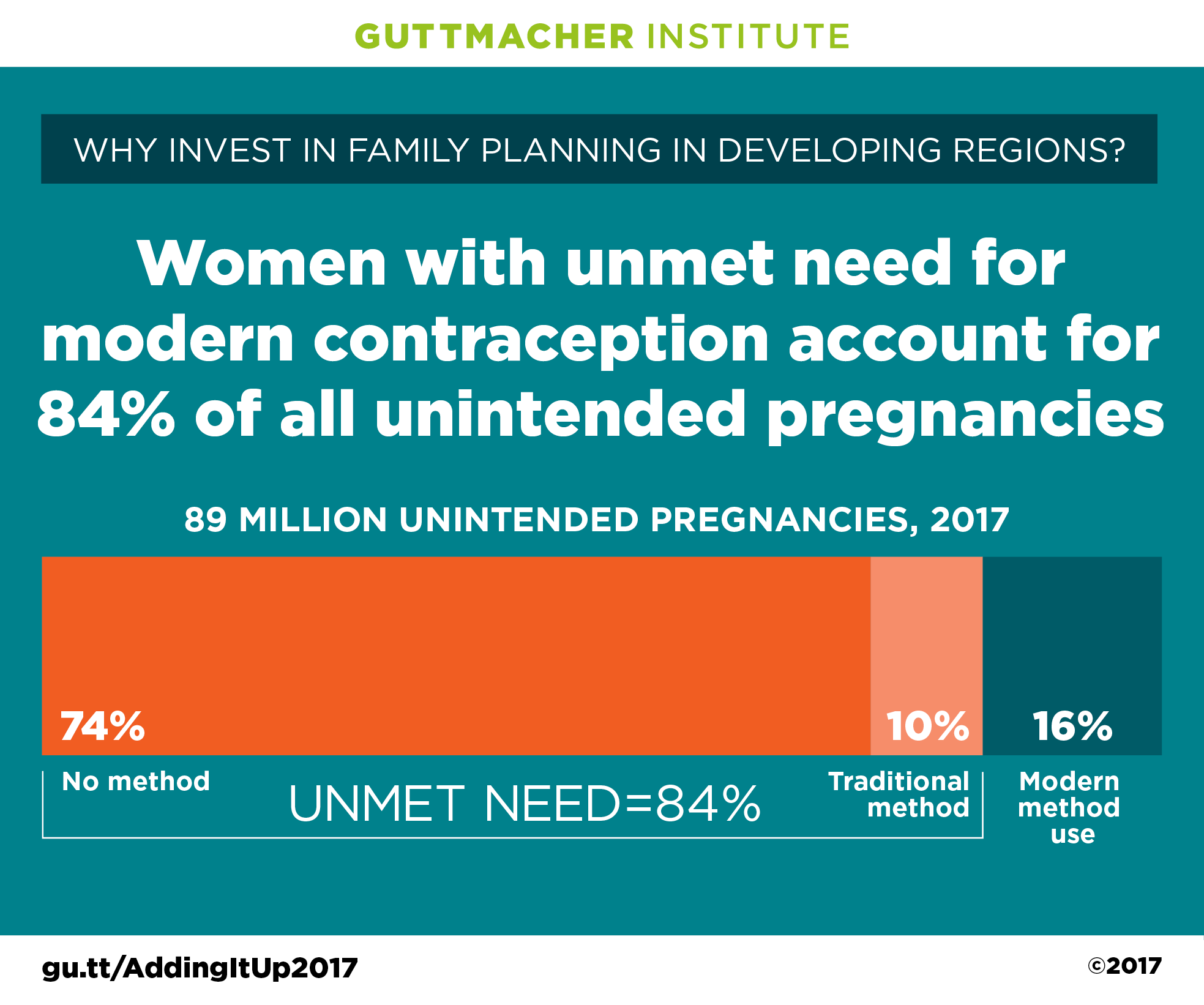
The conscious use of contraception and abortion to control fertility thus assumes paramount importance in explaining basic aspects of contemporary human society. However, substantial differences exist in fertility and contraceptive levels and access to services between developed and developing regions of the world.
For example, while in more developed regions women now have fewer than two children on average and nearly 7 in 10 women in marital or consensual unions use contraceptives (mainly sterilization, the pill, or the male condom), women in Africa have about five children on average and fewer than 3 in 10 women in marital or consensual unions use contraceptives (mainly the pill, injectables, and implants) (United Nations 2004).
Other factors such as social structure, culture, gender relations, and economic opportunities also con tribute to these regional differences.
The area of sexual and reproductive health is broad and encompasses sexual behavior (as it relates to marriage, pregnancy, and fertility; adolescents’ sexual activity;
and risky sexual behaviors that can lead to unintended pregnancy, sexually transmitted infections (STIs) and the human immunodeficiency virus (HIV));
STIs and other reproductive tract infections (the prevention, diagnosis, and treatment of these infections);
contraceptive use (measuring the demand for and effective use of contraceptive methods, reasons for non-use, and method choice and discontinuation);
abortion (levels of and access to abortion, unsafe abortion and its consequences, and post abortion care);
reproductive morbidities (e.g., infertility and reproductive cancers, obstetric fistula, and con sequences of female genital cutting);
contraceptive and abortion technology (the feasibility, acceptability, and demand for new methods such as medical abortion, female condoms, microbicides, and various male contraceptive methods);
family planning related information and education (including sex education in schools and condom promotion); and reproductive health care (e.g., financing, access to, and quality of reproductive health care and its effects on reproductive outcomes).
Studies tend to have close ties to health policies and programs and focus on levels, determinants, and consequences of family planning, abortion, and sexual and reproductive health related problems. Sources of evidence have changed immensely over time, moving from a heavy reliance on indirect estimates based on census data to population based surveys (from the 1970s onward) and clinic based studies to the use of qualitative evidence (from the 1990s onward), mainly from focus group discussions, in depth interviews, and ethnographies.
Research and public policy emphases up until the early 1990s were grounded in arguments for reducing population growth, and the areas of abortion and reproductive health were not very visible.
The 1994 International Conference on Population and Development (ICPD) in Cairo, Egypt, and its final document, the Program of Action, shifted the focus from overpopulation concerns and demo graphic targets to an emphasis on reproductive rights.
An example of this shift is reflected in the increasing use of the concept of ‘‘unmet need for family planning,’’ which includes both contraceptive behavior and fertility preferences and reflects the situation of individuals who want to avoid or delay a birth but who are not using any method of contraception, as a justification for and indicator of family planning program efforts and needs (Casterline & Sinding 2000).
Understanding why people are in this apparently paradoxical situation and how best to meet their contraceptive needs adheres to the overall approach of satisfying individual reproductive choice rather than meeting national targets. Recent studies point to lack of knowledge about contraceptive methods, social opposition to contraceptive use, and concerns about health side effects as important reasons for why women and men do not use contraceptives though they want to delay or avoid pregnancy (Casterline & Sinding 2000).
The ICPD conference also expanded sexual and reproductive health to encompass a broad set of issues beyond family planning, such as women’s rights to control their sexuality.
Sub sequent policymaking, advocacy, and scholar ship turned to gender inequities that affect key determinants of sexual and reproductive health. The often unstated assumption that women hold full decision making power over their health has been supplanted by research on the influence of spouses, parents, and peers, gender based power and violence in sexual relationships, women’s status and access to resources, and neighborhood and community level characteristics.
For example, while a community based family planning program in Ghana led to increased contraceptive use, there were related strains in gender relations in the communities and fears among women of beatings by their husbands if they used contraceptives (Bawah et al. 1999). There is also increased attention to how voluntary sexual intercourse is, especially for young women, and the implications of these findings for women’s rights as well as sexual and reproductive health.

Several studies in developed and developing countries show evidence that women who experience sexual or physical abuse (in childhood or in relationships as adults) are also more likely to experience STIs, pelvic inflammatory disease, and unwanted fertility (Jejeebhoy & Koenig 2003).
Broadening the interpretation of reproductive health to include more than family planning has been supported by the dramatic spread of HIV/AIDS since the 1980s.
The epidemic has spurred research on male condom use for HIV and STI prevention, including investigations of the barriers to consistent and correct use of condoms and women’s difficulties in negotiating condom use, and has legitimated the study of sexual behavior as it relates to sexual and reproductive health.
Issues that continue to plague researchers and program planners alike include the difficulty of increasing condom use (especially within marriage), how protection from disease is reconciled with planning births, and how the nature of reproductive decision making has changed in the context of HIV/AIDS, especially for people who are HIV positive.
Historically, women’s experiences dominated research studies and data on family planning, abortion, and reproductive health, since women were deemed more accurate reporters of reproductive events and perceived as the people ‘‘at risk.’’
Many data collection efforts in the 1960s were limited to married women and then expanded in the 1970s, and later in some regions, to include unmarried women. Evidence on men’s sexual and reproductive health is mainly from the 1990s and 2000s.
A recent worldwide study documented that men are involved in family planning decisions – many have discussed family planning with their partners and used methods to space or limit births – and many men who have an STI say they have informed their partners of the infection or have sought treatment (Alan Guttmacher Institute 2003).
Nevertheless, established family planning and reproductive health care services are much better developed for women in most countries (though there are still subgroups of women who are underserved) than for men.
Recent research incorporates men’s views and experiences by studying couples and their reproductive behaviors. Studies of couples reflect the broader social context in which decisions like contraceptive use are made, and evidence shows that partners have significant influence over one another’s contraceptive behavior via their individual fertility preferences and approval of and communication about family planning.
Couple studies have tended to focus on contraceptive use (including condom use for preventing STIs), and much less on abortion or other sexual and reproductive health outcomes.
One methodological challenge which arises is when partners have different reports of the same behavior. For example, men have been shown to report much higher levels of condom use than do women, both in the aggregate and within couples.
Abortion remains one of the more difficult topics to study despite its widespread practice – estimates suggest that about one quarter of pregnancies worldwide end in abortion – because of the moral arguments surrounding abortion, the criminalization of the practice in many countries, and the clandestine nature of abortion for many women and abortion providers. Measuring the extent of abortion and abortion related complications, particularly in countries where abortion is illegal and records are not maintained at health facilities, is critical to understanding the magnitude of the public health impact of abortion.
Methods to measure the prevalence of abortion include records from registration systems (based on reports from hospitals, clinics, and private doctors), surveys of abortion providers, and surveys of women in the community.
Other techniques, such as third party reports, where women report on abortions they know other women in the community or in their social networks have had, have also been used. Most evidence is on the level of abortion and much less on reasons why women obtain abortions and the social, health, and economic consequences of unsafe abortion.
Monitoring changes in public opinion toward abortion, especially the conditions under which it should be legal, is also important given links between popular acceptance of abortion and the politics of its legal status. Yet even abortion attitudes are difficult to measure; for example, more people in the United States agree that abortion should be legal for any reason when a survey question specifies a first trimester pregnancy than when no pregnancy gestation is stated (Bumpass 1999).
With the continued decline of fertility worldwide, persistent inequities in sexual and reproductive health (including access to services), and the spread of HIV/AIDS, questions about the ways that women and men – as individuals and as partners in sexual relationships – can better achieve their childbearing desires and protect their sexual and reproductive health become increasingly important to address.
Future directions for social research will include a focus on the contextual factors that shape individuals’ use of contraception, abortion, and reproductive health services; the continued inclusion of men in analyses of sexual and reproductive health; understanding the barriers to effective contraceptive use; ways to increase the dual use of contraceptive methods for pregnancy and STI prevention; the conditions under which risky or coercive sex occurs; greater attention to sexual and reproductive decision making; and new techniques to improve reporting of sexual behavior and abortion.
For more such notes, Articles, News & Views Join our Telegram Channel.
Click the link below to see the details about the UPSC –Civils courses offered by Triumph IAS. https://triumphias.com/pages-all-courses.php