Radioactive medications target cancer with accuracy
Why in News
On a Wednesday morning in late January 1896, a significant medical breakthrough occurred at a small light bulb factory in Chicago. Rose Lee, a middle-aged woman with a tumor in her left breast, became the first patient to receive X-ray therapy. This marked the beginning of a journey in cancer treatment that has evolved dramatically over the years. Today, tumor-seeking radiopharmaceuticals are revolutionizing oncology, offering targeted treatments with fewer side effects.
The Evolution of Radiation Therapy Radiation therapy has advanced significantly since its inception. The discovery of radium and other radioactive metals enabled higher doses of radiation to target deeper cancers. Proton therapy later allowed precise targeting of tumors, minimizing damage to healthy tissues. However, the advent of targeted radiopharmaceuticals in the new millennium brought molecular precision to cancer treatment.

The Rise of Targeted Radiopharmaceuticals Targeted radiopharmaceuticals work like heat-seeking missiles, traveling through the bloodstream to deliver radioactive particles directly to tumor sites. Currently, only a few of these therapies are commercially available, primarily for prostate cancer and neuroendocrine tumors. However, this number is set to grow as major biopharmaceutical companies invest heavily in this technology.
Major Investments in Radiopharmaceuticals In recent years, companies like AstraZeneca, Bristol Myers Squibb, and Eli Lilly have made significant investments in radiopharmaceuticals. These billion-dollar transactions highlight the growing recognition of the potential of these therapies to treat cancer in a fundamentally different way.
Challenges in Manufacturing and Distribution Despite their promise, radiopharmaceuticals present unique challenges. Their manufacturing and distribution must be meticulously timed to ensure the radioactive particles remain potent when they reach the patient. Expanding these therapies to treat a broader range of cancers will require developing new tumor-killing particles and finding additional suitable targets.
Atomic Advances in Cancer Treatment For decades, radioactive iodine was the only radiopharmaceutical available, primarily used to treat thyroid cancer. However, researchers have developed drugs that target specific proteins made by tumor cells, delivering radioactive isotopes directly to the cancer site. Initially, these drugs were used for imaging, but they have evolved to include more potent radioactive payloads aimed at killing cancer cells.
Early Successes and Setbacks The first radiopharmaceutical therapy, Quadramet, was approved in 1997 but was not widely adopted. Two drugs for lymphoma in the early 2000s also faced challenges despite showing promise in clinical trials. These early setbacks slowed investment in radiopharmaceuticals, but ongoing research at universities kept the field alive.
Breakthroughs in PSMA-Targeted Therapies Researchers at Weill Cornell Medicine developed PSMA-targeted therapies for prostate cancer, delivering radioactive particles directly to the genetic core of tumor cells. These efforts laid the groundwork for a new generation of radiopharmaceuticals.
Lutathera and Novartis’s Commitment Lutathera, a drug targeting somatostatin receptors in neuroendocrine tumors, marked a significant breakthrough. Approved in 2017, it demonstrated the potential of radiopharmaceuticals to slow tumor progression. Novartis’s acquisition of Advanced Accelerator Applications and Endocyte signaled a renewed interest in this field.
The Success of Pluvicto Pluvicto, a PSMA-targeted therapy for advanced prostate cancer, has shown remarkable efficacy, doubling the average time before disease progression and extending patients’ lifespans. This success has positioned Pluvicto as a potential blockbuster therapy.
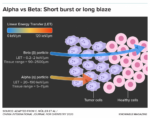
The Future of Alpha-Emitting Radiopharmaceuticals Current research is focusing on alpha-emitting isotopes, which offer highly localized cellular destruction. These isotopes penetrate only a short distance, sparing nearby healthy cells. Companies like Convergent and Fusion Pharmaceuticals are developing innovative alpha-emitting therapies.
Challenges and Opportunities Developing effective radiopharmaceuticals requires finding new cancer-specific targets. While PSMA and somatostatin receptors have been successful, the search for additional targets continues. Novartis and other companies are expanding their manufacturing capabilities to meet the growing demand for these therapies.
ConclusionThe field of radiopharmaceuticals is rapidly evolving, offering new hope for targeted cancer treatments with fewer side effects. As research and investment continue, the potential for these therapies to revolutionize oncology is immense.
FAQs
What are radiopharmaceuticals?
Radiopharmaceuticals are drugs that deliver radioactive particles directly to tumor sites, providing targeted cancer treatment.
What makes radiopharmaceuticals different from traditional radiation therapy?
Radiopharmaceuticals offer molecular precision, targeting specific proteins on tumor cells and minimizing damage to healthy tissues.
Which cancers are currently treated with radiopharmaceuticals?
Currently, radiopharmaceuticals are primarily used for prostate cancer and neuroendocrine tumors.
What are alpha-emitting isotopes?
Alpha-emitting isotopes are radioactive particles that cause highly localized cellular destruction, offering precise cancer treatment.
What challenges do radiopharmaceuticals face?
Radiopharmaceuticals face challenges in manufacturing and distribution, as their radioactive particles must remain potent when administered to patients.
Sociology Optional Program for
UPSC CSE 2025 & 2026
 |
 |
 |
 |
 |
 |
Follow us :
🔎 https://www.instagram.com/triumphias


